Can an Online Doctor Prescribe Adderall?
Most online doctors are unable to prescribe Adderall.
Adderall is classified as a controlled substance by the Food and Drug Administration, and not all online doctors can prescribe controlled substances. For this reason, it is generally recommended to meet with a doctor in person to get an Adderall prescription.
While you can't get Adderall from one of our board-certified doctors online, you may be able to get other ADHD medications with a video or phone appointment.
Here's what you need to know about Adderall, ADHD, and getting prescriptions online.
Book an appointmentCan You Get an Adderall Prescription Online?
As mentioned above, it is not always possible to get an Adderall prescription online.
Why? Because it's a controlled substance due to its addictive nature and the increased risk for abuse. Controlled substances like Adderall are generally only prescribed by a doctor after an in-person visit.
However, there are many other ADHD medications you can request from our doctors online, such as Strattera; its generic version, atomoxetine; guanfacine; and bupropion.
These non-stimulant medications take a few weeks to start working but may treat ADHD as effectively as Adderall without the risk of addiction.
Talk to one of our trusted, board-certified doctors to get these non-stimulant ADHD medications online.
Even though our board-certified doctors cannot prescribe Adderall, we still want to inform you of its uses, side effects, and role in treating ADHD.

1
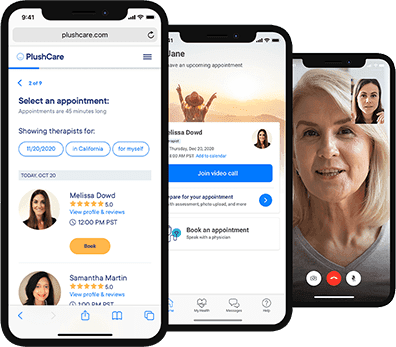
Book on our free mobile app or website.
Our doctors operate in all 50 states and same day appointments are available every 15 minutes.
2
See a doctor, get treatment and a prescription at your local pharmacy.
3
Use your health insurance just like you normally would to see your doctor.
What Does Adderall Treat?
Adderall, which is a combination of amphetamine and dextroamphetamine, is primarily used to treat attention deficit disorder (ADHD). It can also be used to treat narcolepsy.
Adderall Side Effects
Aside from the risk of addiction, Adderall has many potential side effects, including:
Dry mouth
Headache
Nervousness
Nausea
Diarrhea
Constipation
Weight loss
Painful menstrual cramps
Changes in sex drive or ability
Dizziness
Depression
Teeth grinding
Seizures
Mania (frenzied or abnormally excited mood)
Hives
Rash
Itching
Swelling of the tongue, throat, eyes, or face
Blurred vision
Hallucinations
Heart attack
Stroke
Sudden death
Adderall Precautions and Interactions
Adderall isn't right for everybody. Always tell your doctor about your complete health history and any medications you take, including supplements and over-the-counter medications.
Be especially sure to mention any of the following health conditions:
Glaucoma
Anxiety
Irregular heartbeat
Heart attack
Hyperthyroidism
Heart disease
Depression, bipolar disorder, or another mental illness
Seizures
Kidney or liver disease
Pregnant, breastfeeding, or may become pregnant
Also tell your doctor if you take any of the following:
Monoamine oxidase (MAO) inhibitors
Alpha-blockers
Antacids and other medications for heartburn or ulcers
Antidepressants
Antihistamines
Ascorbic acid (Vitamin C)
Beta-blockers
Buspirone
Chlorpromazine
Fentanyl
Lithium
Meperidine
Methenamine
Medications for migraine headaches
Medications for seizures
Quinidine
Reserpine
Ritonavir
Selective serotonin reuptake inhibitors
Serotonin and norepinephrine reuptake inhibitors
Sodium bicarbonate
Sodium phosphate
Thiazide diuretics (water pills)
Tramadol
St. John's wort
Tryptophan
glutamic acid (L-glutamine)
ADHD Diagnosis
An ADHD diagnosis is typically made after getting a history of symptoms, using symptom checklists, and ruling out physical causes for the symptoms.
ADHD Treatment
ADHD is treated with medication, therapy, or both.
Talk therapy is about discussing how ADHD affects you or your child's life and coming up with ways to manage it.
Behavior therapy focuses on monitoring and changing behavior to manage ADHD.
Stimulant medications like Adderall and Ritalin increase the amount of dopamine and norepinephrine in the brain. They work quickly but carry a high risk of addiction and side effects. Stimulant medications are controlled substances and can only be prescribed during in-person doctor appointments.
Non-stimulant medications, usually antidepressants, can also be used to treat ADHD. While the medications take a few weeks to build up in the system and start reducing symptoms, they are generally considered safer than stimulants and can be prescribed online.
Frequently Asked Questions
Can I Get Adderall without Health Insurance?
Yes, you can get Adderall without health insurance. However, the name brand is very expensive, more than $200 for 30 capsules.
Can You Get Generic Adderall?
Yes, you can get generic Adderall for a reasonable price, under $30 in some cases.
Can Adderall Be Prescribed Electronically?
Since Adderall is a controlled substance, it is recommended that you must see a doctor in person for a prescription.
Can I Get Treated for ADHD Online?
Yes, non-stimulant ADHD medications can be prescribed after an online appointment.
If you'd like to talk about non-stimulant medication for ADHD, our licensed doctors can provide you with more information. They'll ask about your symptoms, medical history, and any medications you may be taking.
If they think you would benefit from a non-stimulant ADHD medication, they can electronically send it to your pharmacy.
Make an online doctor appointment below, or download the PlushCare mobile app.

1
Book on our free mobile app or website.
Our doctors operate in all 50 states and same day appointments are available every 15 minutes.
2
See a doctor, get treatment and a prescription at your local pharmacy.
3
Use your health insurance just like you normally would to see your doctor.
Therapy may also help treat the symptoms of ADHD. Now, you can get online therapy with PlushCare. To schedule an appointment for online therapy, click below.
1
Browse our network of top therapist to find one that matches your needs.
2
Get private and secure emotional support weekly from your dedicated therapist.
3
Experience comprehensive care with unlimited access to your care team and primary care physician.
Read More About ADHD Treatment
Sources:
PlushCare is dedicated to providing you with accurate and trustworthy health information.
Medline Plus. Dextroamphetamine and Amphetamine. Accessed on December 10, 2020 at https://medlineplus.gov/druginfo/meds/a601234.html
Centers for Disease Control and Prevention. What Is ADHD? Accessed on December 10, 2020 at https://www.cdc.gov/ncbddd/adhd/facts.html
National Institute of Mental Health. Attention-Deficit/Hyperactivity Disorder. Accessed on December 10, 2020 at https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd/index.shtml



