- Chronic Care
- Heart Disease
Antiarrhythmics
Antiarrhythmic prescriptions available online
Learn how antiarrhythmics can help cardiac arrhythmias with a consultation from one of our trusted doctors online. Get a new prescription or refill for antiarrhythmics from a board-certified doctor online.
Book an appointmentOnline, same-day doctor appointment booking
Available nationwide, with licensed medical providers
Insurance accepted, but not required
Save up to 80% on your prescriptions* with RX discount card
*Prescriptions are provided at the doctor’s discretion. Learn more about our controlled substances policy and our prescription discount card.
Most major insurance plans accepted
Most patients with in-network insurance pay $30 or less. Paying without insurance? New patient visits are $129, and follow-ups are only $99 for members.
Don’t see your provider listed? Email [email protected] or call (888) 564-4454 to talk to a PlushCare specialist.
3 simple steps to getting antiarrhythmics online

Step 1
Book an appointment to discuss antiarrhythmics.
Book a same day appointment from anywhere.
Step 2
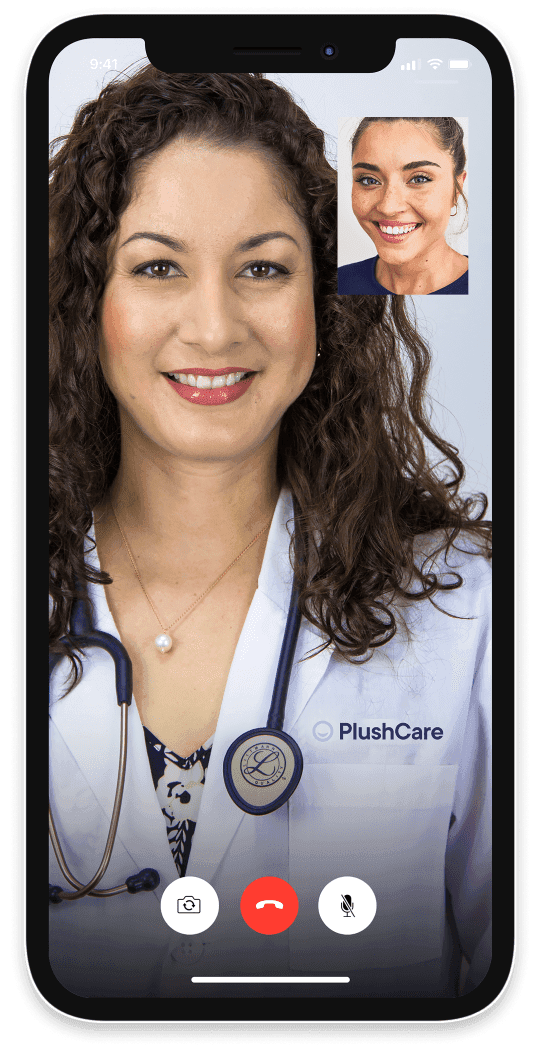
Talk to your doctor online about antiarrhythmics.
See a doctor on your smartphone or computer.
Step 3
Pick up your antiarrhythmics prescription.
We can send antiarrhythmics to any local pharmacy.
Antiarrhythmics pricing details
How pricing works
To get antiarrhythmics online, join our monthly membership and get discounted visits.
Paying with insurance
Membership
$14.99/month
First month free
First visit
Copay
For all visits
30 days of free membership
Same-day appointments 7 days a week
Unlimited messages with your Care Team
Prescription discount card to save up to 80%
Exclusive discounts on lab tests
Free memberships for your family
Cancel anytime
Visit price with insurance
Often the same as an office visit. Most patients with in-network insurance pay $30 or less!
We accept these insurance plans and many more:
Paying without insurance
Membership
$14.99/month
First month free
First visit
$129
Repeats only $99
30 days of free membership
Same-day appointments 7 days a week
Unlimited messages with your Care Team
Prescription discount card to save up to 80%
Exclusive discounts on lab tests
Free memberships for your family
Cancel anytime
Visit price without insurance
Initial visits are $129 and follow-ups are only $99 for active members.
If we're unable to treat you, we'll provide a full refund.
Antiarrhythmic FAQs
How should I take antiarrhythmics?
Always take antiarrhythmic drugs as prescribed by your doctor. Don't stop taking any prescription medication without consulting your healthcare provider. If you experience any side effects after starting antiarrhythmic drugs, make sure to tell your doctor.
Many rhythm disorders, including ventricular tachycardia, respond to antiarrhythmic drugs. Although antiarrhythmic medications can't cure an arrhythmia, they can help improve symptoms. It's important to take your arrhythmia medications regularly to prevent future episodes of cardiac arrhythmia.Who shouldn’t take antiarrhythmics?
To make sure antiarrhythmic drugs are safe for you, tell your doctor if you have certain medical conditions, such as:
Allergies to foods or dyes
Left ventricular dysfunction or left ventricular hypertrophy
Asthma or other breathing problems, such as COPD or lung disease
Thyroid problems
Liver disease
Kidney disease
Lupus
If you're pregnant or planning to become pregnant
What to assess before taking antiarrhythmics?
Your healthcare provider will assess your apical pulse rate and rhythm before prescribing an antiarrhythmic.
In addition, your healthcare provider will regularly monitor your cardiac rate and rhythm after you start antiarrhythmic drug therapy or any time the dosage is adjusted. You may also need regular blood tests to monitor your liver, thyroid, lung, and renal function.What is the most common side effect of antiarrhythmics?
The most common side effects of antiarrhythmic drugs are tiredness and nausea. Side effects are common with antiarrhythmic medications, so it's important to pay attention to any side effects and talk about them with your healthcare provider. For many people, side effects gradually decrease over the course of a few weeks.
What effects do antiarrhythmics have on the heart?
Antiarrhythmic drugs help manage electrical impulses in your heart, which can cause irregular heart rhythms like atrial fibrillation or tachycardias (fast heartbeats).
Depending on your medical condition, your heart may beat too quickly, too slowly, or erratically (regularly). Arrhythmia medications treat abnormal heart rhythms by stopping extra electrical impulses and preventing abnormally fast electrical impulses from traveling along the heart's tissue.What is the safest antiarrhythmic?
The safest antiarrhythmic will depend on your medical condition and history. Your doctor will help you choose the safest antiarrhythmic for you.
Studies suggest that Tikosyn (dofetilide) and Nexterone (amiodarone) therapy are safe and effective in patients with heart failure. Compared to other antiarrhythmic drugs, Tambocor (flecainide) and Rythmol SR (propafenone) have fewer side effects.How long does it take for antiarrhythmics to work?
It takes one to three weeks for antiarrhythmics to start working, and it can take up to several months for an antiarrhythmic to take full effect. If your doctor prescribes an antiarrhythmic, they may recommend taking it daily and indefinitely to prevent future episodes of cardiac arrhythmia.
What should I avoid with antiarrhythmics?
Avoid drinking alcohol while you're taking an antiarrhythmic. Alcohol can lead to an increased risk of arrhythmia episodes. If you're taking blood thinners for blood clots or high blood pressure, alcohol can also increase your risk of bleeding.
Talk to your doctor before consuming grapefruit or grapefruit juice. Grapefruit may enhance drug toxicity for certain antiarrhythmic medications, including Nexterone (amiodarone) and Coreg (carvedilol), which can lead to adverse reactions.

About antiarrhythmics
Antiarrhythmics, also known as antiarrhythmic agents, are a diverse group of medications used to treat cardiac arrhythmias (abnormal heart rates or rhythms). They're often prescribed to treat different types of arrhythmias, including atrial arrhythmias and ventricular arrhythmias. Antiarrhythmic medications may be prescribed to treat atrial fibrillation, atrial flutter, ventricular tachycardia, or ventricular tachycardia. There are four types of antiarrhythmics.
What antiarrhythmics treat
The most common condition treated with antiarrhythmics is cardiac arrhythmias or heart rhythm disorders. Irregular heartbeats may be used by a congenital condition or may develop if part of the heart muscle becomes irritated or damaged, leading to a "short circuit" in the heart's electrical system. Arrhythmia medications are designed to slow the electrical impulses in the heart, allowing the heart to resume regular rhythm control.
Other conditions are also treated with antiarrhythmics. For example, antiarrhythmic drugs may be used to treat arrhythmias associated with coronary artery disease, heart attacks, electrolyte imbalances, structural heart disease, or infections by restoring the heart's normal rhythm.
Types of antiarrhythmics available online
The four types of antiarrhythmic medications are called sodium channel blockers, beta-blockers, potassium channel blockers, and calcium channel blockers.
Class I sodium channel blockers
Sodium channel blockers, or class I agents, prevent sodium from entering cell membranes by creating a sodium channel blockade. This helps slow electrical impulses in the heart muscle. Sodium channel blockers can help treat atrial fibrillation, ventricular fibrillation, and other types of arrhythmias.
Examples of sodium channel blockers include:Dilantin (phenytoin)
Tambocor (flecainide)
Rythmol SR (propafenone)
Class II beta-blockers
Beta-blockers, or class II agents, block the electrical impulses that may cause an irregular heart rhythm. They also interfere with hormonal imbalances, such as adrenaline, in the heart's cells. By doing this, beta-blockers help lower blood pressure, reduce heart rate, and lower the risk of blood clots.
Examples of beta-blockers include:Class III potassium channel blockers
Potassium channel blockers, or class III agents, prevent potassium from entering cell membranes, which prolongs the repolarization of the cell membrane. In turn, this can slow down electrical impulses in the heart's cells.
Examples of potassium channel blockers include:Class IV calcium channel blockers:
Calcium channel blockers, or class IV agents, work similarly to class III agents. However, instead of blocking potassium channels, calcium channel blockers block calcium channels in the heart. This reduces the movement of calcium ions in the heart cells.
Examples of calcium channel blockers include:Cartia XT (diltiazem)
Calan SR (verapamil)
How antiarrhythmics work
Antiarrhythmics are part of a heart rhythm control strategy. They work to reset your heart to a normal rhythm or prevent episodes of cardiac arrhythmia. Different types of arrhythmia medications work on the heart's electrical system to stop extra electrical impulses or prevent abnormally fast electrical impulses from traveling along the heart tissue.
Most people take arrhythmic drug therapy orally over a long period of time to prevent future episodes of cardiac arrhythmia. If you're unable to take oral medications, some arrhythmia drugs can also be delivered intravenously (injected into the bloodstream) by a healthcare provider.
Side effects of antiarrhythmics
When taken as prescribed, antiarrhythmics are generally well tolerated. However, they can still cause some side effects. The more common side effects of antiarrhythmics include:
Constipation
Dizziness
Excessive thirst
Nausea
Swelling (fluid retention)
Vision changes
Urinary retention
In rare cases, antiarrhythmic therapy may cause serious side effects. These can include:Shortness of breath
Heart palpitations
Low blood sugar
Depression, confusion, or hallucinations
Sudden or severe chest pain
Antiarrhythmic risks
Antiarrhythmic medication is generally safe, but there are some risks if you have other medical conditions or take certain medications. Before you take prescribed antiarrhythmic drug therapy, be sure to tell your doctor if you have any of the following conditions or issues:
Allergies to foods or dyes
Asthma or other breathing problems, such as COPD or lung disease
Left ventricular dysfunction or left ventricular hypertrophy
Thyroid problems
Liver disease
Kidney disease
Lupus
If you're pregnant or planning to become pregnant
Antiarrhythmic drug interactions
When you begin a new medication, make sure to tell your doctor about any other medications, supplements, or over-the-counter medications you’re taking. Some medications that might interact with antiarrhythmic medications include:
Cholestyramine or colestipol
Other heart or blood pressure medications
Antibiotic or antifungal medicines
Nonsteroidal anti-inflammatory drugs, such as naproxen (Aleve), ibuprofen (Advil), and aspirin
Steroid medicine
Certain antidepressant medications
Coumadin (warfarin)
PlushCare online antiarrhythmics ratings and reviews
Our online doctors have treated over 550,000 patients.